"Rozplątywanie zapalenia: Obrońca, który stał się sprawcą w chorobach przewlekłych"
01. Zgłębianie zapalenia i układu odpornościowego
Wprowadzenie i Przegląd
Zapalenie jest podstawową reakcją układu odpornościowego organizmu mającą na celu ochronę przed szkodami, takimi jak infekcje, urazy i toksyny, inicjując proces gojenia. Choć zazwyczaj korzystne w sytuacjach ostrych, gdy zapalenie staje się przewlekłe, może prowadzić do poważnych konsekwencji zdrowotnych, przyczyniając się do szeregu chorób, w tym chorób serca, cukrzycy i raka. Zrozumienie dwoistej natury zapalenia — jego roli zarówno w ochronie, jak i potencjalnym szkodzeniu organizmowi — jest kluczowe dla zarządzania zdrowiem i zapobiegania chorobom.
"Wyjaśnienie zapalenia"
Zapalenie to reakcja układu odpornościowego na szkodliwe bodźce, charakteryzująca się zaczerwienieniem, ciepłem, obrzękiem, bólem i utratą funkcji. Proces ten jest niezbędny dla mechanizmów gojenia i obrony organizmu, obejmując złożoną sieć cząsteczek sygnałowych i komórek, które działają w celu wyeliminowania przyczyny uszkodzenia komórek, usunięcia martwych komórek i zainicjowania naprawy tkanek. Jednak gdy zapalenie utrzymuje się poza początkową reakcją na uraz lub infekcję, może stać się przewlekłe i przyczynić się do postępu różnych chorób.
Głębsze zrozumienie roli zapalenia w naprawie ran ujawniło zarówno korzystne, jak i szkodliwe efekty. Badania wyjaśniły molekularne i komórkowe mechanizmy kontrolujące zapalenie w naprawie tkanki skórnej, podkreślając znaczenie ukierunkowania fazy zapalnej w celu modulacji wyniku gojenia. Na przykład, Eming, Krieg i Davidson (2007) podkreślili kluczową rolę zapalenia w ustanawianiu homeostazy skórnej po urazie, ale także potencjał zapalenia do opóźniania gojenia i zwiększania bliznowacenia, wskazując na złożoność wpływu zapalenia na naprawę tkanki (Eming, Krieg, & Davidson, 2007).
"Twój układ odpornościowy wyjaśniony"
Układ odpornościowy to zaawansowany mechanizm obronny, który chroni organizm przed zagrożeniami zewnętrznymi, takimi jak bakterie, wirusy i toksyny, a także przed zagrożeniami wewnętrznymi, jak komórki rakowe. Składa się z dwóch głównych komponentów: wrodzonego układu odpornościowego, który zapewnia natychmiastową, ale niespecyficzną obronę, oraz adaptacyjnego układu odpornościowego, który zapewnia ukierunkowaną odpowiedź na określone patogeny. Układ wrodzony jest pierwszą linią obrony i odpowiada za początkową reakcję zapalną. W przeciwieństwie do niego, układ adaptacyjny obejmuje tworzenie komórek pamięci, które rozpoznają i reagują bardziej efektywnie na wcześniej napotkane patogeny.
Proces zapalny jest integralną częścią funkcjonowania układu odpornościowego, ułatwiając usuwanie szkodliwych bodźców i inicjując naprawę tkanek. Kluczowymi uczestnikami procesu zapalnego są białe krwinki (leukocyty), takie jak makrofagi i neutrofile, które pochłaniają i niszczą patogeny. Cytokiny, białka sygnałowe uwalniane przez komórki, odgrywają kluczowe role w mediacji i regulacji odpowiedzi zapalnej.
W kontekście gojenia się ran, zapalenie jest pierwszym krokiem, po którym następuje tworzenie się tkanek i ich przebudowa. Regulacja zapalenia przez układ odpornościowy jest złożona, z równowagą między sygnałami prozapalnymi a przeciwzapalnymi, co zapewnia prawidłowe gojenie. Nadmierne lub przedłużające się zapalenie może zakłócić tę równowagę, prowadząc do upośledzonego gojenia się ran i przewlekłego zapalenia, co podkreśla znaczenie zrozumienia i potencjalnej modulacji odpowiedzi immunologicznej w celu promowania zdrowia i zapobiegania chorobom.
Złożona relacja między stanem zapalnym a układem odpornościowym jest kluczowa dla zdolności organizmu do samoleczenia i obrony. Badania nadal odkrywają zawiłości tej relacji, dążąc do wykorzystania korzystnych aspektów stanu zapalnego w procesie leczenia, jednocześnie łagodząc jego szkodliwe skutki.
W następnych rozdziałach zbadamy, jak zapalenie przechodzi od mechanizmu ochronnego do potencjalnego czynnika patogennego w różnych chorobach oraz jakie ma to implikacje dla strategii leczenia i zapobiegania.
02. Kiedy dobra zapalenie staje się zła
Wprowadzenie
Podczas gdy stan zapalny jest ochronną i leczniczą reakcją organizmu na uraz lub infekcję, może stać się szkodliwy, gdy utrzymuje się poza swoją użyteczną fazą. Przewlekły stan zapalny leży u podstaw wielu chorób, które dotykają ludzi, od chorób sercowo-naczyniowych po raka i inne. Ta zmiana z korzystnego na szkodliwy stan podkreśla złożoną rolę stanu zapalnego w zdrowiu i chorobie.
Problem zapalny
Przewlekłe zapalenie jest cichym, ale potężnym czynnikiem w rozwoju różnych chorób. Działa poprzez różne mechanizmy, w tym trwałą aktywację szlaków zapalnych, produkcję cząsteczek zapalnych oraz rekrutację komórek odpornościowych, które zamiast rozwiązywać stan zapalny, przyczyniają się do uszkodzenia i dysfunkcji tkanek. Ten trwały stan zapalny może prowadzić do uszkodzenia DNA, promować proliferację komórek, hamować apoptozę (zaprogramowaną śmierć komórki) oraz wspierać angiogenezę (tworzenie nowych naczyń krwionośnych), co wszystko może stworzyć podłoże dla rozwoju raka i innych chorób przewlekłych.
Jednym z godnych uwagi przykładów jest związek między przewlekłym stanem zapalnym a chorobami sercowo-naczyniowymi, metabolicznymi i nerkowymi. Manabe (2011) podkreśla, jak przewlekły stan zapalny wywołany otyłością w tkance tłuszczowej odgrywa kluczową rolę w rozwoju niewydolności serca i przewlekłej choroby nerek, podkreślając wzajemne powiązania chorób przewlekłych poprzez procesy zapalne (Manabe, 2011).
Ponadto, Furman et al. (2019) omawiają, w jaki sposób czynniki społeczne, środowiskowe i styl życia mogą sprzyjać systemowemu przewlekłemu zapaleniu (SCI), prowadząc do chorób, które łącznie stanowią główne przyczyny niepełnosprawności i śmiertelności na całym świecie, takich jak choroby sercowo-naczyniowe, rak, cukrzyca, przewlekła choroba nerek, niealkoholowa stłuszczeniowa choroba wątroby oraz choroby autoimmunologiczne i neurodegeneracyjne (Furman et al., 2019).
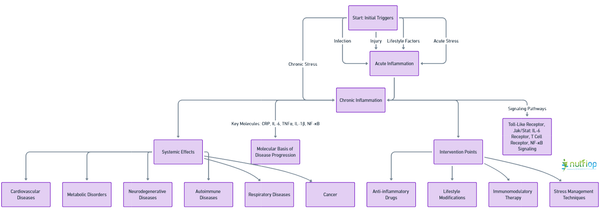
Interaktywny Wykres Chorób
Ten interaktywny wykres chorób ilustruje ścieżki, przez które przewlekłe zapalenie przyczynia się do szerokiego zakresu chorób. Pokazuje, jak początkowe czynniki wyzwalające, takie jak infekcja, uraz lub czynniki związane ze stylem życia, mogą przekształcić się w stan przewlekłego zapalenia, przedstawiając skutki dla różnych układów ciała i podkreślając potencjalne punkty interwencji w celu zapobiegania postępowi choroby.
Quiz sekcji 2
1. Prawda czy Fałsz: Ostre zapalenie zawsze prowadzi do przewlekłego zapalenia.
2. Która z poniższych chorób nie jest zazwyczaj związana z przewlekłym stanem zapalnym?
a. Cukrzyca typu 2
b. Choroba Alzheimera
c. Ostre zapalenie wyrostka robaczkowego
d. Rak
3. Jaką rolę odgrywa otyłość w przewlekłym zapaleniu?
a. Nie ma wpływu na stan zapalny.
b. Zmniejsza przewlekłe zapalenie.
c. Powoduje przewlekłe miejscowe zapalenie w tkance tłuszczowej.
d. Natychmiast łagodzi stany zapalne.
4. Który z poniższych czynników nie sprzyja przewlekłemu zapaleniu ogólnoustrojowemu (SCI)?
a. Uszkodzenie ciała
b. Zła dieta
c. Regularne ćwiczenia
d. Stres psychologiczny
Kliknij tutaj, aby ujawnić odpowiedzi.
Odpowiedzi: 1. Fałsz, 2. c, 3. c, 4. c
Zrozumienie przejścia od korzystnego ostrego zapalenia do szkodliwego przewlekłego zapalenia dostarcza kluczowych informacji na temat mechanizmów chorobowych i oferuje potencjalne strategie wczesnej diagnozy, zapobiegania i leczenia. Poprzez zajęcie się podstawowymi przyczynami i procesami przewlekłego zapalenia, możliwe jest złagodzenie jego wpływu na szeroki wachlarz chorób przewlekłych.
03. Zapalenie i reakcje alergiczne
Wprowadzenie
Alergiczne zapalenie to złożona odpowiedź immunologiczna wywołana ekspozycją na alergeny. W przeciwieństwie do korzystnego zapalenia, które wspomaga gojenie, alergiczne zapalenie jest nadmierną reakcją układu odpornościowego na nieszkodliwe substancje, takie jak pyłki, roztocza kurzu czy niektóre pokarmy. Ta nadmierna reakcja może prowadzić do różnych chorób alergicznych, w tym kataru siennego, egzemy i astmy, dotykając znaczną część populacji na całym świecie.
Alergie i zapalenia
Proces zapalenia alergicznego obejmuje aktywację różnych komórek układu odpornościowego, takich jak komórki tuczne, eozynofile i limfocyty T. Po ekspozycji na alergen, osoby z nadwrażliwością produkują przeciwciała Immunoglobuliny E (IgE), które wiążą się z receptorami na komórkach tucznych i bazofilach. To wiązanie wyzwala uwalnianie histaminy i innych mediatorów zapalnych, prowadząc do objawów takich jak obrzęk, zaczerwienienie i swędzenie. Rola IgE i komórek tucznych w inicjowaniu reakcji alergicznych podkreśla złożony związek między układem odpornościowym a alergenami (Barnes, 2011).
Egzema i astma
Egzema (atopowe zapalenie skóry) i astma to przewlekłe schorzenia charakteryzujące się alergicznym stanem zapalnym. Egzema objawia się swędzącą, zapalną skórą, podczas gdy astma wpływa na drogi oddechowe, prowadząc do trudności w oddychaniu. Oba schorzenia są napędzane przez odpowiedzi immunologiczne typu 2, z udziałem komórek Th2 i cytokin takich jak IL-4 i IL-13, które promują produkcję IgE i aktywację eozynofili. Wzajemne oddziaływanie między wrodzonymi i adaptacyjnymi odpowiedziami immunologicznymi, z udziałem komórek takich jak komórki tuczne, bazofile i grupy 2 wrodzonych komórek limfoidalnych (ILC2s), odgrywa kluczową rolę w patologii tych chorób (Kubo, 2017).
Leczenie
Zarządzanie stanem zapalnym związanym z alergią polega przede wszystkim na unikaniu znanych alergenów oraz stosowaniu leków w celu kontrolowania objawów. Kortykosteroidy są skuteczne w redukcji stanu zapalnego, podczas gdy leki przeciwhistaminowe mogą łagodzić swędzenie i obrzęk poprzez blokowanie działania histaminy. W przypadku przewlekłych schorzeń, takich jak astma i ciężkie alergie, można zastosować immunoterapię, aby stopniowo odczulać układ odpornościowy na określone alergeny.
Quiz sekcji 3
1. Które komórki odpornościowe odgrywają kluczową rolę na początku reakcji alergicznej?
A) Limfocyty B
B) Komórki tuczne i eozynofile
C) Czerwone krwinki
D) Płytki krwi
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: B) Komórki tuczne i eozynofile
Wyjaśnienie:
Komórki tuczne i eozynofile odgrywają kluczową rolę w początkowych etapach reakcji alergicznej. Po ekspozycji na alergen, te komórki są aktywowane i uwalniają mediatory zapalne, takie jak histamina, co prowadzi do typowych objawów alergicznych.
2. Jaka jest funkcja cytokin Th2 w kontekście chorób alergicznych, takich jak egzema i astma?
A) Zmniejszają produkcję IgE.
B) Ułatwiają aktywację komórek Th1.
C) Promują produkcję IgE i aktywację eozynofili.
D) Hamują degranulację komórek tucznych.
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: C) Promują produkcję IgE i aktywację eozynofili.
Wyjaśnienie:
Cytokiny Th2, w tym IL-4 i IL-13, odgrywają kluczową rolę w napędzaniu odpowiedzi immunologicznych typu 2, charakterystycznych dla stanów alergicznych, poprzez promowanie produkcji IgE i aktywację eozynofili. To nasila alergiczne zapalenie obserwowane w egzemie i astmie.
3. Opisz rolę immunoglobuliny E (IgE) w zapaleniu alergicznym.
A) Wiąże się z antygenami, aby zapobiec reakcjom alergicznym.
B) Jest produkowany w odpowiedzi na bodźce niealergiczne.
C) Wiąże się z receptorami na komórkach tucznych i bazofilach, wywołując uwalnianie mediatorów zapalnych.
D) Dezaktywuje eozynofile i zmniejsza stan zapalny.
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: C) Wiąże się z receptorami na komórkach tucznych i bazofilach, wyzwalając uwalnianie mediatorów zapalnych.
Wyjaśnienie:
IgE odgrywa centralną rolę w reakcjach alergicznych. Osoby z alergiami produkują przeciwciała IgE, które wiążą się z receptorami na komórkach tucznych i bazofilach. Ta interakcja powoduje, że komórki uwalniają różne mediatory zapalne, prowadząc do objawów alergicznych.
4. Jakie są skuteczne strategie leczenia w zarządzaniu zapaleniem alergicznym?
A) Zwiększenie narażenia na alergeny
B) Stosowanie kortykosteroidów i leków przeciwhistaminowych
C) Podawanie antybiotyków
D) Unikanie leków przeciwzapalnych
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: B) Stosowanie kortykosteroidów i leków przeciwhistaminowych.
Wyjaśnienie:
Zarządzanie stanem zapalnym związanym z alergią często polega na unikaniu znanych alergenów oraz stosowaniu leków w celu kontrolowania objawów. Kortykosteroidy zmniejszają stan zapalny, podczas gdy leki przeciwhistaminowe łagodzą swędzenie i obrzęk poprzez blokowanie działania histaminy. W przypadku przewlekłych lub ciężkich alergii można również rozważyć immunoterapię, aby stopniowo odczulać układ odpornościowy na określone alergeny.
Zrozumienie mechanizmów zapalenia alergicznego jest kluczowe dla opracowywania ukierunkowanych terapii w celu skutecznego leczenia i zapobiegania chorobom alergicznym. Badania nadal odkrywają złożone interakcje między komórkami układu odpornościowego, mediatorami a czynnikami środowiskowymi w reakcjach alergicznych, dając nadzieję na nowe i ulepszone metody leczenia.
04. Zapalenie i choroby autoimmunologiczne
Wprowadzenie
Choroby autoimmunologiczne powstają, gdy układ odpornościowy błędnie atakuje własne komórki organizmu, prowadząc do przewlekłego stanu zapalnego i różnych problemów zdrowotnych. Te schorzenia mogą dotyczyć niemal każdej części ciała, w tym stawów, skóry, mózgu i narządów wewnętrznych, powodując szeroki zakres objawów i komplikacji.
Kiedy Twoje Ciało Walczy z Samym Sobą
Patogeneza chorób autoimmunologicznych obejmuje złożoną interakcję między predyspozycjami genetycznymi a czynnikami środowiskowymi, prowadzącą do załamania tolerancji immunologicznej. Centralną rolę w tym procesie odgrywa zapalenie, które nie tylko stanowi odpowiedź na uszkodzenie tkanek, ale w kontekście chorób autoimmunologicznych przyczynia się do uszkodzenia tkanek. Na przykład mutacja typu gain-of-function w fosfolipazie C gamma 2 może powodować ciężkie spontaniczne zapalenie i autoimmunizację poprzez zwiększenie zewnętrznego napływu Ca2+, co podkreśla genetyczne podstawy takich chorób (Yu et al., 2023). Podobnie, dysregulowane szlaki receptorów Toll-podobnych (TLR), które są kluczowe dla odporności wrodzonej, zostały powiązane z różnymi chorobami autoimmunologicznymi, co podkreśla rolę odpowiedzi immunologicznych wrodzonych w rozwoju autoimmunizacji (Chen, Szodoray, & Zeher, 2016).
Zwalczanie zapalenia
Zarządzanie stanem zapalnym jest kluczowe w leczeniu i zarządzaniu chorobami autoimmunologicznymi. Strategie obejmują stosowanie leków przeciwzapalnych, immunosupresantów oraz biologicznych środków celujących w specyficzne szlaki immunologiczne zaangażowane w proces zapalny. Na przykład, przeciwciała monoklonalne celujące w TNF-alfa, cytokinę znacząco zaangażowaną w mediację ogólnoustrojowego stanu zapalnego, okazały się skuteczne w leczeniu chorób takich jak reumatoidalne zapalenie stawów i choroba Crohna. Ponadto, zrozumienie wpływu mikrobiomu na odpowiedzi immunologiczne oferuje nowe możliwości interwencji terapeutycznych, ponieważ zmiany w mikrobiocie jelitowej zostały powiązane z wieloma schorzeniami autoimmunologicznymi (Wu, Zegarra-Ruiz, & Diehl, 2020).
Quiz sekcji 4
1. Co inicjuje atak układu odpornościowego na własne komórki organizmu w chorobach autoimmunologicznych?
A) Zewnętrzne patogeny, takie jak bakterie i wirusy
B) Załamanie tolerancji immunologicznej z powodu czynników genetycznych i środowiskowych
C) Bezpośrednie uszkodzenie tkanek i organów
D) Nadmierna produkcja czerwonych krwinek
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: B) Załamanie tolerancji immunologicznej z powodu czynników genetycznych i środowiskowych.
Wyjaśnienie:
Choroby autoimmunologiczne występują, gdy dochodzi do niepowodzenia w tolerancji immunologicznej, co prowadzi do tego, że układ odpornościowy błędnie atakuje własne komórki organizmu. Ta złożona interakcja między predyspozycjami genetycznymi a czynnikami środowiskowymi skutkuje przewlekłym stanem zapalnym i uszkodzeniem tkanek.
2. Jaką rolę odgrywa stan zapalny w rozwoju i postępie chorób autoimmunologicznych?
A) Sygnałuje organizmowi, aby produkował więcej białych krwinek.
B) Działa wyłącznie jako reakcja ochronna na uraz.
C) Przyczynia się do uszkodzenia tkanek i zaostrza chorobę.
D) Nie ma znaczącego wpływu na choroby autoimmunologiczne.
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: C) Przyczynia się do uszkodzenia tkanek i zaostrza chorobę.
Wyjaśnienie:
W kontekście chorób autoimmunologicznych, zapalenie nie jest tylko reakcją na uszkodzenie tkanek, ale centralnym czynnikiem przyczyniającym się do uszkodzenia tkanek. Przewlekłe zapalenie napędzane aktywnością autoimmunologiczną pogarsza stan i może prowadzić do różnych powikłań.
3. Jaką rolę odgrywają czynniki genetyczne w rozwoju chorób autoimmunologicznych?
A) Mają mniejszy wpływ w porównaniu do wyborów stylu życia.
B) Predyspozycje genetyczne mogą znacząco wpływać na ryzyko rozwoju chorób autoimmunologicznych.
C) Tylko czynniki środowiskowe są odpowiedzialne za choroby autoimmunologiczne.
D) Czynniki genetyczne wpływają jedynie na ciężkość, a nie na prawdopodobieństwo wystąpienia chorób autoimmunologicznych.
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: B) Predyspozycje genetyczne mogą znacząco wpływać na ryzyko rozwoju chorób autoimmunologicznych.
Wyjaśnienie:
Czynniki genetyczne odgrywają kluczową rolę w chorobach autoimmunologicznych, predysponując jednostki do wyższego ryzyka rozwoju tych schorzeń. Chociaż czynniki środowiskowe również są istotne, to podstawa genetyczna może determinować podatność na reakcje autoimmunologiczne.
4. Dlaczego zarządzanie stanem zapalnym jest ważne w leczeniu chorób autoimmunologicznych?
A) Zapalenie nie odgrywa roli w chorobach autoimmunologicznych i nie wymaga zarządzania.
B) Zmniejszenie stanu zapalnego może złagodzić objawy i zapobiec dalszemu uszkodzeniu tkanek.
C) Zarządzanie stanem zapalnym pomaga jedynie w poprawie fizycznego wyglądu objawów.
D) Zarządzanie stanem zapalnym jest konieczne tylko w początkowych stadiach chorób autoimmunologicznych.
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: B) Zmniejszenie stanu zapalnego może złagodzić objawy i zapobiec dalszemu uszkodzeniu tkanek.
Wyjaśnienie:
W chorobach autoimmunologicznych zarządzanie stanem zapalnym jest kluczowe, ponieważ pomaga złagodzić objawy i zapobiega dalszym uszkodzeniom tkanek spowodowanym przewlekłymi reakcjami zapalnymi. Skuteczne zarządzanie stanem zapalnym jest istotnym elementem strategii leczenia, poprawiającym jakość życia osób dotkniętych tymi chorobami.
Złożona relacja między stanem zapalnym a autoimmunizacją podkreśla znaczenie zrozumienia regulacji układu odpornościowego oraz czynników prowadzących do jego dysregulacji. Postępy w badaniach genetycznych i biologii molekularnej nadal odkrywają złożoność chorób autoimmunologicznych, obiecując bardziej ukierunkowane i skuteczne terapie w zarządzaniu stanem zapalnym i autoimmunizacją. (Yu et al., 2005), (Chen, Szodoray, & Zeher, 2016), (Wu, Zegarra-Ruiz, & Diehl, 2020).
05. Wpływ zapalenia na organizm
Wprowadzenie
Przewlekłe zapalenie jest coraz częściej uznawane za kluczowy czynnik w rozwoju szerokiego zakresu chorób. Podczas gdy ostre zapalenie jest istotną częścią mechanizmu obronnego organizmu, przewlekłe zapalenie może prowadzić do szkodliwych skutków w różnych układach narządów, przyczyniając się do patogenezy licznych chorób związanych z wiekiem i metabolicznych, a także nowotworów.
Serce
Przewlekłe zapalenie odgrywa kluczową rolę w rozwoju chorób sercowo-naczyniowych. Przyczynia się do powstawania blaszek miażdżycowych, które mogą prowadzić do zawałów serca i udarów mózgu. Cytokiny zapalne i komórki biorą udział we wszystkich etapach miażdżycy, od początkowego uszkodzenia śródbłonka po ostateczne pęknięcie blaszki. Obecność ogólnoustrojowego przewlekłego zapalenia (SCI) jest również wskaźnikiem złych rokowań u pacjentów z chorobami sercowo-naczyniowymi, co podkreśla potrzebę strategii zarządzania zapaleniem w celu zmniejszenia ryzyka sercowo-naczyniowego (Furman et al., 2019).
Mózg
Zapalenie jest również zaangażowane w kilka chorób neurodegeneracyjnych, takich jak choroba Alzheimera i choroba Parkinsona. Przewlekłe zapalenie może zaostrzać neurodegenerację poprzez aktywację mikrogleju, rezydentnych komórek odpornościowych mózgu, prowadząc do uwalniania prozapalnych cytokin i substancji neurotoksycznych. Ten proces zapalny przyczynia się do postępu neurodegeneracji i klinicznych objawów tych chorób.
Choroby metaboliczne
Przewlekłe zapalenie jest kluczowym czynnikiem prowadzącym do insulinooporności i cukrzycy typu 2. Zapalenie tkanki tłuszczowej, w szczególności, odgrywa istotną rolę w rozwoju zespołu metabolicznego. Cytokiny zapalne zakłócają sygnalizację insuliny, co prowadzi do upośledzonego wchłaniania glukozy i zwiększonego ryzyka cukrzycy. Zarządzanie stanem zapalnym poprzez interwencje związane ze stylem życia, takie jak dieta i ćwiczenia, może poprawić wrażliwość na insulinę i pomóc w kontrolowaniu chorób metabolicznych.
Rak
Zapalenie przyczynia się do inicjacji, progresji i przerzutów nowotworu. Komórki zapalne i cytokiny w mikrośrodowisku guza promują wzrost guza, angiogenezę oraz tłumienie odpowiedzi immunologicznej przeciwko guzowi. Przewlekłe zapalenie może również prowadzić do uszkodzenia DNA, co przyczynia się do mutagenezy inicjującej rozwój nowotworu. Strategie ukierunkowane na szlaki zapalne są badane jako potencjalne terapie w zapobieganiu i leczeniu nowotworów.
Quiz sekcji 5
1. W jaki sposób przewlekłe zapalenie przyczynia się do rozwoju chorób układu sercowo-naczyniowego?
A) Poprzez obniżenie poziomu cholesterolu
B) Poprzez promowanie powstawania blaszek miażdżycowych
C) Poprzez poprawę funkcji śródbłonka
D) Poprzez obniżenie ciśnienia krwi
Kliknij tutaj, aby ujawnić odpowiedź.
Prawidłowa odpowiedź:: B) Poprzez promowanie powstawania blaszek miażdżycowych
Wyjaśnienie:
Przewlekłe zapalenie jest kluczowym czynnikiem w rozwoju chorób sercowo-naczyniowych, głównie poprzez swoją rolę w promowaniu powstawania blaszek miażdżycowych. Te blaszki mogą prowadzić do zawałów serca i udarów mózgu poprzez zwężanie i twardnienie tętnic.
2. W jaki sposób zapalenie jest zaangażowane w choroby neurodegeneracyjne, takie jak choroba Alzheimera?
A) Chroniąc neurony przed uszkodzeniem
B) Poprzez promowanie neurogenezy
C) Poprzez aktywację mikrogleju i uwalnianie prozapalnych cytokin
D) Poprzez poprawę funkcji synaptycznej
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: C) Poprzez aktywację mikrogleju i uwalnianie cytokin prozapalnych
Wyjaśnienie:
Zapalenie odgrywa istotną rolę w chorobach neurodegeneracyjnych, takich jak choroba Alzheimera, poprzez aktywację mikrogleju, rezydentnych komórek odpornościowych mózgu. Prowadzi to do uwalniania prozapalnych cytokin i substancji neurotoksycznych, co zaostrza neurodegenerację i przyczynia się do postępu choroby.
3. Opisz rolę zapalenia w zespole metabolicznym i cukrzycy typu 2.
A) Zwiększa wrażliwość na insulinę
B) Promuje insulinooporność
C) Zwiększa wychwyt glukozy w tkankach
D) Zmniejsza tkankę tłuszczową
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: B) Promuje insulinooporność.
Wyjaśnienie:
Przewlekłe zapalenie jest kluczowym czynnikiem prowadzącym do insulinooporności, będącej cechą charakterystyczną zespołu metabolicznego i cukrzycy typu 2. Cytokiny zapalne, szczególnie pochodzące z tkanki tłuszczowej, zakłócają sygnalizację insuliny, co prowadzi do upośledzonego wchłaniania glukozy i zwiększonego ryzyka rozwoju tych chorób metabolicznych.
4. Wyjaśnij związek między przewlekłym stanem zapalnym a rakiem.
A) Zapalenie zmniejsza wzrost guza i przerzuty
B) Komórki zapalne i cytokiny w mikrośrodowisku guza hamują rozwój raka
C) Przewlekłe zapalenie może prowadzić do uszkodzenia DNA i promować wzrost guza, angiogenezę oraz supresję układu odpornościowego.
D) Zapalenie wzmacnia zdolność układu odpornościowego do celowania i niszczenia komórek rakowych.
Kliknij tutaj, aby ujawnić odpowiedź.
Poprawna odpowiedź:: C) Przewlekłe zapalenie może prowadzić do uszkodzenia DNA i promować wzrost guza, angiogenezę oraz supresję układu odpornościowego.
Wyjaśnienie:
Przewlekłe zapalenie przyczynia się do inicjacji, progresji i przerzutów nowotworów. Komórki zapalne i cytokiny w mikrośrodowisku guza wspierają wzrost i przeżycie guza, promują rozwój nowych naczyń krwionośnych (angiogenezę) oraz tłumią odpowiedź immunologiczną przeciwko guzowi, ułatwiając tym samym progresję nowotworu.
Przewlekłe zapalenie jest wspólnym wątkiem łączącym wiele chorób, co podkreśla znaczenie zarządzania stanem zapalnym w celu poprawy wyników zdrowotnych. Zrozumienie mechanizmów, dzięki którym zapalenie przyczynia się do chorób, może pomóc w opracowaniu ukierunkowanych terapii mających na celu złagodzenie jego szkodliwych skutków. (Furman et al., 2019)


